SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan
sOAP Notes 2
SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan. The episodic SOAP note is to be written using the attached template below.Graduate SOAP NOTE TEMPLATE.docx
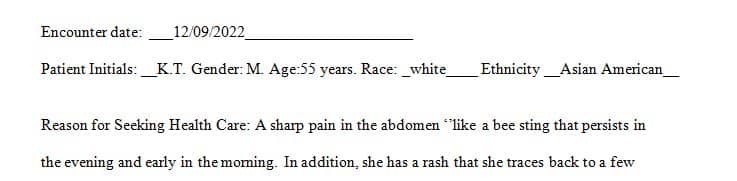
For all the SOAP note assignments, you will write a SOAP note about one of your patients and use the following acronym:
S =
Subjective data: Patient’s Chief Complaint (CC).
O =
Objective data: Including client behavior, physical assessment, vital signs, and meds.
A =
Assessment: Diagnosis of the patient\’s condition. Include differential diagnosis.
P =
Plan: Treatment, diagnostic testing, and follow up
Submission Instructions:
- Your SOAP note should be clear and concise and students will lose points for improper grammar, punctuation, and misspelling.
- Complete and submit the assignment using the appropriate template in MS Word
- •Please note, You must receive a Turnitin similarity report that is less than or equal to 20% in order to post to the Discussion board.
- Your instructor will monitor your similarity report and you will automatically receive a 0 in the discussion if you post with a Turnitin similarity report that is greater than 20%.
Answer preview to SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan
APA
1963 words
